On August 16, 2019, Netflix aired a new documentary series Diagnosis. The second episode, titled Second Opinions, features a couple from Queens whose otherwise typically-developing seven-year-old daughter Sadie has started having seizures. Members of our parent and medical community have expressed concern about the misinformation provided in this episode. Our response is below and includes important points to clarify several incorrect statements made in the show.
The Episode
After several different tests, we’re told that Sadie’s first medical team proposed that she has Rasmussen’s encephalitis, an extremely rare, progressive neurological condition characterized by brain atrophy, seizures, progressive neurological dysfunction, hemiparesis, and cognitive decline.
However, because magnetic resonance imaging of Sadie’s brain did not reveal the typical marker of Rasmussen’s encephalitis – progressive cerebral atrophy – Sadie’s parents seek a second opinion on diagnosis. The episode then follows her parents’ quest to find the correct diagnosis for Sadie.
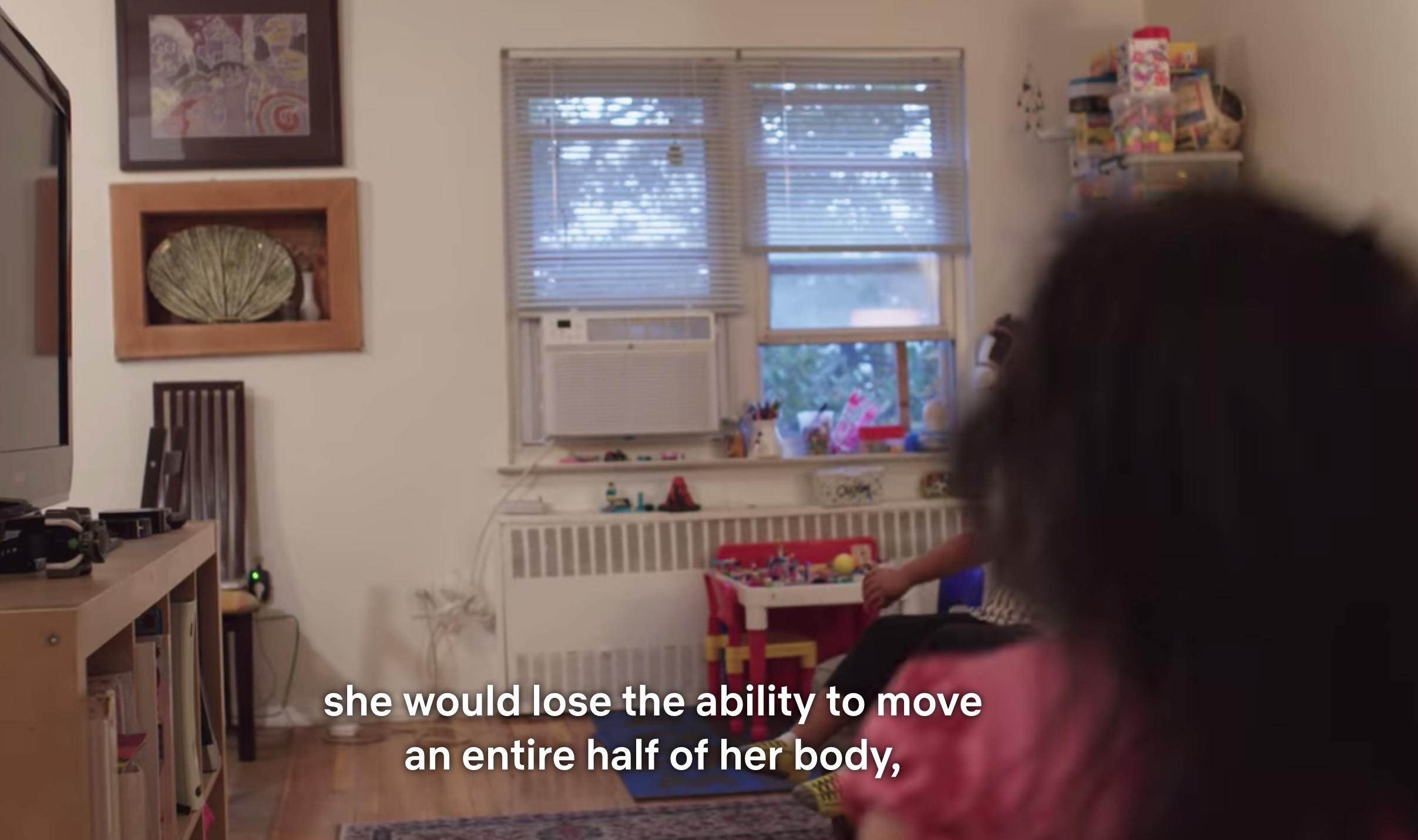
If the diagnosis is in fact Rasmussen’s encephalitis, we’re told by the host Dr. Lisa Sanders that the only known cure is hemispherectomy – a procedure she calls “devastating”- where half the brain is either removed or disconnected. Dr. Sanders describes that the surgery causes total paralysis on the opposite side of the body and loss of vision in one eye, but that if the child has surgery before age four or five, she would likely recover normal function. Because Sadie is six years old, Dr. Sanders tells us that the opportunity for regaining control of lost functions after surgery has passed.


After the crowd suggests different potential diagnoses, the episode takes a detour by introducing the viewer to a new and exciting treatment – a small device that is implanted into the skull, with leads that are inserted into the brain and uses electrical stimulation to hopefully reduce the amount of Sadie’s seizures.

Compared to hemispherectomy, which is later described as “barbaric”, Sadie’s parents choose the brain implant in the hope that it will stop Sadie’s seizures.
Our Concern
We understand that by framing hemispherectomy as a “barbaric” and “devastating” surgery that it adds a dramatic and sensational hook to the storyline, depicting hemispherectomy as an outrageous choice as compared to a new and untested cutting-edge device. We know that it is an excruciating decision for any parent to choose hemispherectomy as a treatment for one’s child, and we respect Sadie parents’ choice to pursue a different treatment option in light of her unclear diagnosis.
This is an important point to highlight: parents must first obtain a solid diagnosis before choosing hemispherectomy as a treatment option. Sadie does not have one here.
However, because of the way hemispherectomy is portrayed in the program, we are concerned that families considering this surgery will be discouraged or dissuaded from pursuing hemispherectomy as an option after viewing this episode, even though their child may desperately need it. We believe that it is imperative that any parent of a child with a unilateral drug-resistant epilepsy who has been presented with hemispherectomy as a treatment option who have viewed this program makes their decision based on accurate facts.*
Movement and Vision
Hemispherectomy does not result in a total paralysis of the opposite side of the body. This would be truly devastating and make it physically impossible to walk. Rather, hemispherectomy results in a significant weakness on the opposite side of the body, known as hemiparesis, and is most prominent in the hands and feet where fine motor control requires input from the brain via a large tract of neuronal fibers which innervate the many muscles of the hands and feet.
However, while one side of the brain controls most of the movement of the opposite side of the body, there are axons from one side of the brain which go to the large muscles of the legs and arms of the same side of the body, and some to the hands and feet. In other words, the remaining hemisphere has some connection to the same side of the body.
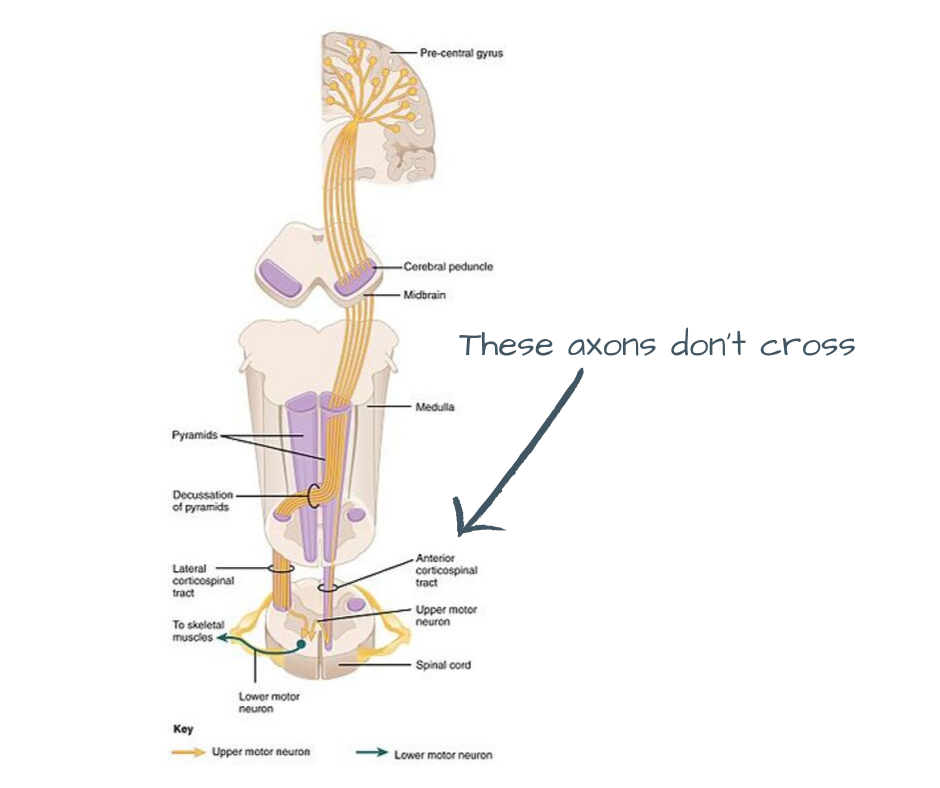
This is why almost 90% of children can walk after hemispherectomy and, remarkably, 25% of children who could not walk prior to surgery can walk after surgery.
Children who undergo hemispherectomy will experience loss of half the vision in both eyes known as homonymous hemianopia, not all vision in one eye. This is important for parents and anyone working with a child after hemispherectomy to understand because it is a more significant vision loss than losing vision in one eye – the vision loss is half the visual field straight down the middle of the visual scene and moves with the eyeballs. However, the children after surgery generally compensate quite well for this vision loss with the help of orientation and mobility specialists and teachers of the visually impaired.
Neuroplasticity
Neuroplasticity is generally described by Dr. Sanders as ending at an arbitrary cut-off date of age four or five. This statement is based on outdated notions of neuroplasticity that have been debunked. Modern theories of neuroplasticity support that the brain changes continuously in response to our actions and experiences, even into adulthood. While it is true that neuroplasticity is stronger in early childhood, there is no magic date when it stops.
Similarly, it’s important for any parent considering hemispherectomy to understand that surgery at a very young age does not guarantee that the brain will reorganize its firing pattern or exploit remaining connections in such a way that all lost functions will be recovered. We know, for example, that the visual field loss regardless of age at surgery is permanent and unavoidable and that fine motor function in the opposite hand is significantly impaired.
What does affect how well a child functions after surgery is a constellation of factors which include, but are not limited to, the length of time the child was seizing prior to surgery, the frequency of the seizures, the type of seizure, whether they occurred in infancy, the nature and extent of the brain malformation or condition which causes the seizures, whether this condition is present in the otherwise healthy side of the brain, whether seizures have caused damage to the healthy hemisphere’s neurons and/or circuitry, how the brain reorganized prior to surgery, how young the child was at the time of the original brain insult, whether seizures after surgery return, and intensity and frequency of physical and other therapies – not just age at the time of surgery.
Most children after hemispherectomy, regardless of the age it was performed, walk after surgery – although with a familiar hemiparetic limp (thus not “completely normally” as stated by Dr. Sanders). And a new, growing body of research shows that harnessing neuroplasticity with intensive physical therapy even years after surgery can improve gait and walking ability.
We have children in our community who had hemispherectomy to the left side of the brain as late as age 12 and are trilingual post-operatively, and others as late as age 19 who go to college and graduate school, are married, have children, and living great lives.
Outcomes after hemispherectomy are not based on an arbitrary cut-off date based on age at the time of surgery, and it would be unfortunate if a parent considering hemispherectomy for their child declined the procedure because the child was older than five.
Treatment
Hemispherectomy is the only research-backed and data-supported option that could achieve seizure freedom and stop the progressive neuropathological features of Rasmussen’s encephalitis, such as brain atrophy, inflammation, gliosis, and cortex destruction. It is important for families of children affirmatively diagnosed with Rasmussen’s encephalitis (unlike Sadie) and who are considering hemispherectomy understand that stopping seizures is only one part of the formula: the treatment must also stop the progressive destruction of the brain, which the featured brain implant does not address.**
Hemispherectomy completes what Rasmussen’s encephalitis will do over time in most cases – destroy the affected hemisphere. While this sounds terrible, the notion of hemispherectomy is to do medically what is going to happen anyway and prevent the effects of repeated seizures on the remaining good hemisphere. And surgery bypasses months or years of destructive seizures which can eventually damage the healthy side of the brain and prevents additional developmental impairment and cognitive deficits.
We agree this is not ideal, which is why we strongly advocate for more research support in the field of rare diseases, especially rare epilepsies such as Rasmussen’s encephalitis. Rasmussen’s encephalitis is a disease that affects an otherwise typically-developing child, and although rare (thankfully) should be something we could identify and treat without the need of surgery if there were sufficient resources and research efforts behind it.
Again, it is unfortunate that the procedure is called “barbaric” in this episode. To the contrary: it is a delicate, extremely sophisticated and technical procedure that is constantly being refined by the dedicated, highly trained, and highly skilled neurosurgeons at some of the country’s top children’s hospitals who perform this surgery. Not just any surgeon can perform hemispherectomy – it is a procedure reserved for only the best. We admire and are grateful for the talented, courageous, and caring pediatric neurosurgeons who have changed the lives of the community of children we serve.
Hemispherectomy is life-saving and life-changing for children with catastrophic epilepsy, especially conditions like Rasmussen’s encephalitis for which there is no other known cure.
This statement is supported by:
RE Children’s Project
The Hemispherectomy Foundation
*The creator of the show, Lightbox Entertainment, states on its website that it is a “multi-platform media company creating high quality, non-fiction content …” Merriam Webster’s dictionary defines nonfiction as “writing or cinema that is about facts.” Despite this, Lightbox has declined our request to correct these misstatements and point to the show’s disclaimer that the series is “to entertain and inform” and not to provide medical advice. We cannot ignore that some viewers will take the host’s statements as fact, especially because the series has the weight of the New York Times and Netflix behind it.
**Rasmussen’s encephalitis is diagnosed in part with magnetic resonance imaging of the brain which monitors for progressive cerebral atrophy. Parents of children with unconfirmed but suspected Rasmussen’s encephalitis should understand that the implant in this series is MRI unsafe, meaning anyone who has had the device implanted cannot be scanned in an MRI machine. At this time, there is no other alternative means of brain imaging that can be used to monitor progression of the disease. The implanted device would need to be removed in order to commence MRI monitoring.
Download our full response: Official Response_ Netflix’ Diagnosis Episode 2 (1)
Episode screen shots used in this post are done so under the Fair Use doctrine.




















Leave A Comment
You must be logged in to post a comment.